Mental health medication 'does not have to be pernicious to creativity'
09 April 2020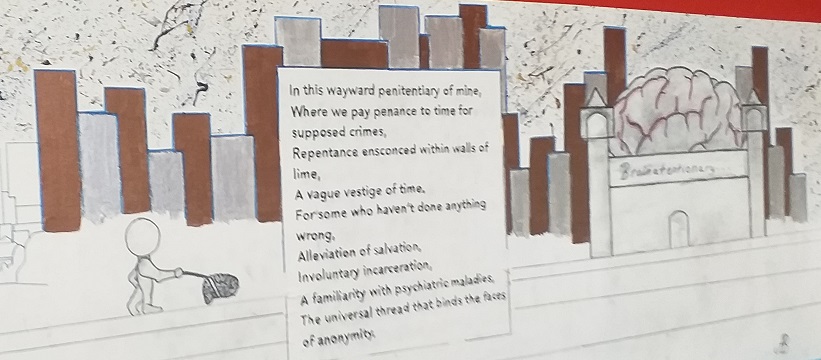
Indefinite isolation is anything but a ‘new normal’ for the thousands of patients diagnosed with mental illnesses cooped up in 60 medium-secure mental health hospitals dotted across England and Wales. The majority know neither when they will be discharged, nor what specifically they need to demonstrate in order to regain their liberty. Mental Health Today spent time with a handful of patients just prior to the wider world falling under a desperate lockdown of its own. This interview is the second instalment of our In Secure series.
Ashley is in his mid-thirties; welcoming, self-assured, immaculately presented, eloquent, calm, inventive, ambitious. He is also in a medium-secure hospital for the forseeable future. And this is not the first one he's spent time in.
"The fact that assessment of health treatment need is made by the government's justice secretary, rather than the health secretary, arguably demonstrates where the state's priorities still rest."
The majority of psychiatric units are low-secure, promoting various freedoms while they treat patients in distress. These patients present a danger to themselves alone and a transient, moderate risk at that. Medium-secure hospitals, in contrast, operate in a similar fashion to Category B prisons. These institutions promise therapeutic intent also. But they are consciously designed with preventing escape as their overriding priority.
Road to rehab
Everyone Ashley lives with on his locked ward has experienced some kind of 'interaction' with the criminal justice system [CJS]. Many are prisoners who have been transferred to hospital as their mental health has deteriorated. Some have never been convicted of a crime but have arrived here having displayed diagnosed symptoms of mental illness during arrest or trial.
"I'm in here on an innocent verdict, but there was violence around the innocent verdict and that's why I got sectioned," Ashley explains. The philosophy graduate distances himself from the profile of others receiving the same medical treatment and psychoeducation he is receiving. "Everyday you're surrounded by people who are just talking about crime and drugs and you're just like, give it a rest, do you know what I mean?"
His hospital support worker, who lives with a bipolar disorder diagnosis herself, insists there is not one 'neat criteria' encompassing everyone who may be admitted for medium-secure care and supervision. "It's not like a lottery where you're the lucky ones who are going to hospital and not staying in prison. It's based on need. So if somebody is really presenting as acutely and severely in distress in a prison environment – and the prison cannot manage that level – and they need a higher level of mental health care, then the hospital environment may be better."
"Prisons are very understaffed as well. If somebody is a real risk to themselves, then a prison environment is not necessarily the best place for them to be because they are locked in. So it's really based on need: who needs that bed."
Soothing or supressing?
The NHS Trust press officer who has arranged the interview interjects to emphase that it "is not just about that [bed provision]. It is about treatment and recovery for the mental health issue as well. So while there is an element about them being in a secure unit so they can't leave and they don't have the limits on their freedom in that way, it is not just about that. It is about recovery and treatment for the illness that perhaps caused the offending, that led them to be involved with the criminal justice system."
Only a tiny proportion of those embroiled in the CJS receive hospital treatment despite some claiming that virtually all prisoners live with diagnosable psychological needs. The fact that assessment of need is made by the government's justice secretary rather than the health secretary arguably demonstrates where the state's priorities still rest.
The context leaves staff having to make up their own minds as to whether they are treating or containing those they are ostensibly 'supporting'. Some are sympathic, others are detached, but the mixed messages inevitably leave patients having to wrestle feeling disenfranchised at times.
"Aleviation from salvation"
Ashley find his current care more therapeutic, "much better", than other hospitals he's been sectioned to in the past. However such are the terms of Section 47 orders that you are obliged to show deference to the state's approach to your mental health. Section 47 orders last three months but they can be extended routinely if the patient doesn't demonstrate sufficient insight, even beyond the end date of a prison sentence.
A poem in Ashley's name that hangs from the wall [pictured above] depicts institutions as coercive, delivering "aleviation from salvation". I ask about the message. "It's the infernal idiocy that you're stooped in most of the time and that [poem] was a reaction to that."
Ashley, who has also published short stories and written film scripts, was encouraged to pursue his creative instincts by Hospital Rooms, an arts charity who support patients to redesign areas of their ward in their own image.
- See also: 'In Secure’: patient portraits – the boxer
- See also: Patient portraits - the painter
The initiative and the approach to medication taken by Ashley's support worker have combined to give him renewed direction and faith in his future prospects, I'm told.
"I'm on fairly positive medication. I'm happy with it given my circumstances. Hospital Rooms inspired me to keep pushing my boundaries and limitations given the implications medication can have for creativity and that's been really a positive aspect."
"Prior to meeting them, my drive for my artistic passions, even though it was there, it was less so that it is now since them having been here."
- Editor's note: do not make changes to your medication without first consulting with your doctor.
Ashley apologies for his medication "making it hard to speak" but he is articulate throughout our discussion. I ask whether, as an expressive person, he carries concerns about his treatment interferring with his ability to channel expansive ideas.
"Not all medication acts that way. There are some medications that are actually quite helpful in that respect. The vast majority, I would say about at least 80 percent, dependent on how you look at it, in terms of antipsychotics, are very pernicious to creativity. It gives you a general sense of lethargy. But on the whole, the other twenty percent, if we can get into that category, they're very good."
"What Hospital Rooms has taught me is that I can recreate the magic that they [showcased in workshops] on a smaller scale myself and then try to propagate that throughout the community in places such as this."
"The most active way of me doing this is through the grant application process that they've schooled me in how to make." Hopefully that will come to fruition. There's no certainty. But if it does, then that will be an active means through which I'll get art out there."
"Then once I get out into the community I'll be able to make grant applications and I've no policies to abide by and so there's the hope of me actually being able to fund myself and make a career as an artist at some level."
The interviewee's name has been changed to protect anonymity of all involved.


Comments
Write a Comment
Comment Submitted